San Antonio Spine Surgeon
Antonio Webb, MD
Dr. Antonio Webb is a board certified and fellowship trained, San Antonio Spine Surgeon who specializes in all medical conditions related to the spine, back and neck including degenerative, deformity, trauma, cervical/lumbar arthroplasty, and minimally invasive spine surgery. Dr. Webb attended the University of Texas at San Antonio (UTSA), Georgetown University medical school and spent his Orthopedic Surgery Residency at UT Health San Antonio. He completed a Spine Surgery fellowship at the Texas Back Institute.
A long-term resident of San Antonio, Texas, Dr. Webb welcomes patients to his clinic who struggle with spine pain and who are looking for a solution. Dr. Webb served eight years in the United States Air Force, including a deployment as a medic to north of Baghdad, Iraq in 2005, before attending college.
“My approach to spine care is empathetic and informative. I see myself as an educator; navigating and empowering my patients to become active decision-makers in their spine care.”
– Dr. Antonio Webb,
Dr. Webb specializes in the treatment of a wide range of conditions related to the cervical, thoracic, and lumbar spine, including deformities and various spine, back, and neck disorders.
Dr. Webb can create a tailored strategy to relieve you from spine, back, and neck discomfort.
Your Spine Health Is Our Top Priority
You Can regain mobility, alleviate pain and improve your overall quality of life.

Artificial Disc Replacement
Fusion Alternative

3D Guided Navigation
Computer Imaging

Augmented Reality
Computer Imaging

Spinal 3D Printing
Patient Specific
Minimally Invasive and
Open Surgery
Specialty Spinal Care

Augmented Reality
Computer Imaging

3D Guided Navigation
Computer Imaging

Spinal 3D Printing
Patient Specific

Minimally Invasive Surgery
Surgery
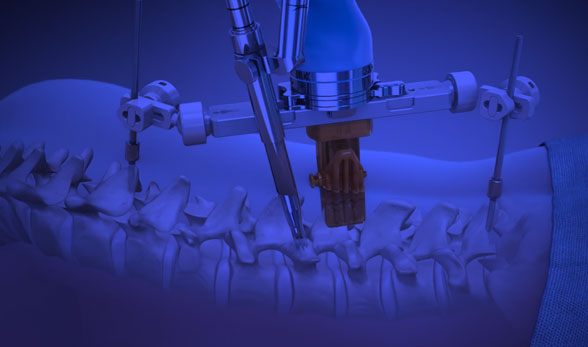
Robotic Spine Surgery
Surgery

Artificial Disc Replacement
Fusion Alternative
Schedule an Appointment Today
San Antonio Area Spine Clinics
Office #1: Medical Center
9150 Huebner Rd. #290,
San Antonio, TX 78240
Office #2: (South) San Antonio
8235 S. New Braunfels Ave #211,
San Antonio, TX 78223
Office #3: New Braunfels
790 Generations Dr. #405,
New Braunfels, TX 78130
Office #4: (North) San Antonio
18626 Hardy Oak Blvd, #300
San Antonio, TX 78258
Orthopedic Spine Surgeon
Memberships
List of Insurances
We Accept
Got a question about your insurance? Please contact us. Click here for a full list of insurances we accept.