What is ACDF?
Anterior is a medical word for “in front”
Cervical is the region of bones that goes from the skull to the bottom of the neck –“ectomy” is a suffix meaning to remove
Fusion is a surgical technique that joins two or more bones in your spine together to eliminate motion.
So an anterior cervical discectomy & fusion is removing the diseased disc from your neck by going through the front and fusing the bones together so that they don’t move. A fusion usually involves placing a bone graft and metal or plastic implant in the space where the disc was removed, in order to provide stability and eliminate motion.
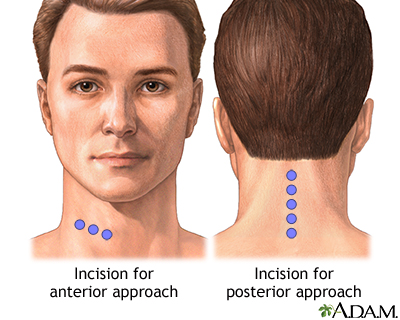
Approach
The surgery is done by making a small incision on either the right side or left side of your neck. This will be decided by Dr. Webb and discussed with you at your visit. Doing the surgery by going through the front of your neck has many advantages over doing the surgery from the back (posterior) of your neck including:
- Lower infection risk vs going through the back of your neck.
- Generally, a quick surgery and shorter recovery than going through the back of your neck.
- Less blood loss
- Less postoperative pain
- Less muscle damage: muscles are not cut, they are moved to the side and allowed to fall back in place when surgery is done.
The Procedure
Anesthesia & Induction
- Your anesthesiologist will talk to you about the specifics of his/her plan for the procedure. You will find out what medications and what type of anesthesia will be used to keep you pain free and comfortable throughout the operation.
- In general, most patients will undergo general anesthesia during spine procedures meaning you will be asleep and wont remember or feel any pain during the procedure itself. Patients may have pain upon waking up from anesthesia, but this will be managed with intravenous and oral pain medications.
- After a breathing tube is placed and you are fully asleep, you will be positioned on the operating room table.
- Surgery will not begin until you are asleep and given pain medications so that you don’t feel any pain during the procedure.
Incision
a. A skin incision is made on the left or right hand side of the anterior neck (depending on surgeon preference). After dissecting through the skin, Dr. Webb will find the space between your esophagus and trachea (windpipe). He will carefully move these out of the way. In between these two structures lies your spine. No muscles are cut, they are just moved to the side and held apart with the use of special tools, called retractors.
Performing the Decompression
- Before removing the diseased disc, Dr. Webb will confirm that he is operating at the correct level by taking an x-ray while you are asleep.
- When the level is confirmed, Dr. Webb will then begin the decompression (removing the areas of compression from your spinal cord) portion of the procedure.
- Dr. Webb will then carefully remove the disc that is pressing on your spinal cord/nerves with the use of special instruments and tools.
- With the diseased disc removed, any additional surrounding structures which may be pressing on your spinal cord and/or spinal nerves, such as bone spurs and/or excess ligaments, will be removed.
- Dr. Webb will then ensure that your spinal cord and nerves are free from compression.
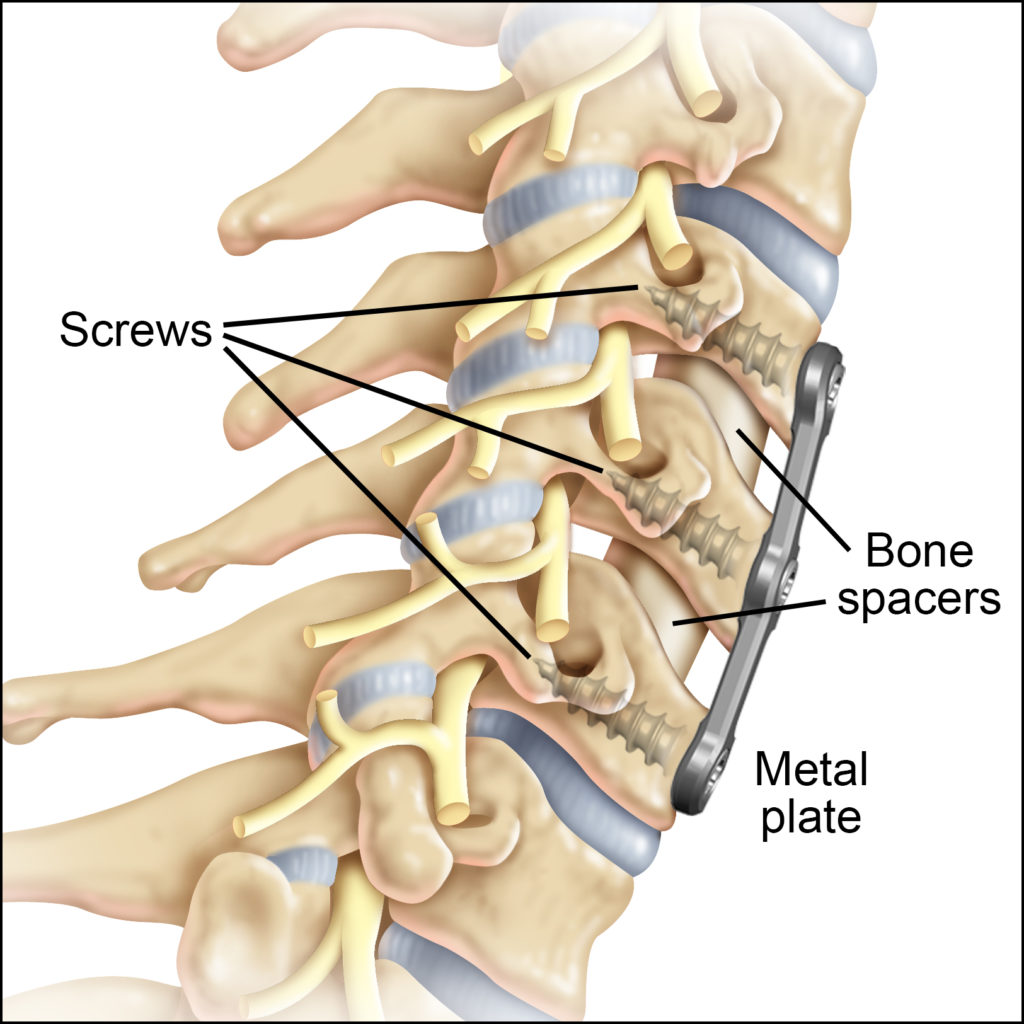
Performing the Fusion
- After the spinal cord has been decompressed and all the diseased disc material removed, this area/void needs to be replaced with something so that it can fuse together.
- This area will now be replaced with bone graft material and a metal or plastic cage.
- The bone graft will help your neck to fuse.
- The metal or plastic cage will indirectly decompress your spinal cord and nerves by “jacking open” your disc space.
- This is similar to “jacking up” and changing your tires on your car after a flat tire. When your car is “jacked up”, there is more room for the tire to be placed and also relieves pressure off of the tire. Similarly, in spine surgery, when a metal or plastic cage is placed in between your bones, this “jacks up” the space that houses your spinal cord and nerves, giving them more room.
- Dr. Webb will then use a small metal plate and screws in order to stabilize and complete the operation.
Closure
- The retractors that held the area between your trachea and esophagus apart will now be removed and the trachea/esophagus will be allowed to fall back into their normal position.
- Dr. Webb uses absorbable sutures to close your wound. These sutures do not typically need to be removed and will absorb on their own.
- Sometimes, a special tube called a drain will be used. This is to collect any blood or fluids that can collect after surgery. This drain will be removed before you leave the hospital, usually the next day after surgery.
“Surgery should only be used as a final and last resort.”
ANTONIO WEBB, MD
What to expect after Surgery
After surgery you will be transferred to the recovery room, also called the PACU (post anesthesia care unit). After you have awaken from the anesthesia, you will then be transferred to your hospital room. This is typically when your family members can visit you.
Either the same day or the following morning after surgery, a physical and/or occupational therapist will begin your therapy. During your hospital stay, you will be given medications to help with pain and IV antibiotics to minimize the risk of infection. Most patients spend 1-2 nights in the hospital and are discharged home after:
- You are tolerating a diet
- Your pain is controlled
- After you have worked with and passed physical therapy.
Walking after surgery is highly encouraged, even the same day of surgery!
Frequently Asked Questions
What kind of recovery can you expect after Surgery?
Recovery from ACDF surgery takes 8-12 weeks for the bones to heal, but most patients continue to heal for up to a year after surgery.
When can I return to work and/or activities?
Walking is highly encouraged, immediately after surgery and throughout your post-operative period. Most patients can return to a light desk job or household activities by 2-3 weeks after surgery. Patients with jobs that require heavy lifting or strenuous labor will not be allowed to return until Dr. Webb ensures your bones have fused. In addition, activities such as biking, skiing, or running will not be allowed until Dr. Webb ensures your bones have fused.
When will my neck or arm pain go away?
If you can imagine putting your elbow on a hard surface for a long time, what happens? Your fingers start to go to sleep. Why? Because the nerves to these fingers is compressed, is asleep, and is irritable. Once you realize this, you pick up your elbow (to remove the pressure off of the nerve) and shake your fingers until they wake up. If you have had compression of your nerves and spinal cord for months to years, then it may take some time before the nerve recovers and wakes up (if it recovers at all). Most patients, however, wake up from surgery with arm pain relief meaning that the debilitating arm pain they had before surgery has went away, but may have some neck pain and spasms from the surgical incision itself. This pain will be controlled with oral/IV pain medications and antispasm medications throughout your hospital stay.
When and how will my bones fuse together?
Once Dr. Webb removes the diseased disc and replaces it with a metal or plastic cage and bone graft, this starts the process of spinal fusion. How quickly your bone fuses depends on many factors such as your bone quality, your general overall health, if you are a smoker or not, etc but most patients can expect a solid fusion by 12 weeks post op.Once Dr. Webb confirms adequate fusion (usually around 3-4 months after surgery), he may then allow you to return to more strenuous activities such as running, biking, etc.
What complications are there with this procedure?
There are risks to any surgery that you should be aware of:
Inadequate relief of symptoms
- Dr. Webb is very particular about making sure we target the right level of your spine that may be causing your symptoms.
- Inadequate relief of symptoms after surgery could be due to a number of things including: multiple levels that are degenerated or worn out that will not be addressed in surgery, surgery done on the wrong level, or advanced and severe spinal cord compression that may be irreversible.
- Injections are confirmatory and are very predictive of how well you will do with surgery. These spinal injections, usually done before surgery in the conservative treatment period, are essential in determining which level of your spine is the cause of your symptoms.
- Multiple degenerated areas of your spine, seen on your imaging studies such as MRI, X-ray, etc., does not mean every level needs an operation. Dr. Webb believes in symptom specific surgery.
Failure of bone graft to heal adequately (called a non-union or pseudarthrosis)
- This risk is elevated if you are a smoker, are older than 60 years old, on chronic steroids, have osteoporosis, history of previous spine surgery, or if you are diabetic.
- Smoking cessation, optimizing your bone and general health, and maintaining normal glucose levels are recommended before any spine procedure to give you the best outcome.
- Some patients whose bones do not fuse after this procedure may require additional surgery to reattempt a spinal fusion, if their symptoms are bad enough to warrant it.
Nerve damage, causing speech or swallowing issues
- There are small nerves that control your larynx (voice box) that reside very close to the surgical site.
- Dr. Webb carefully works around these nerves and ensures they are not damaged during surgery.
- If they become irritated by surgery, your voice may be hoarse for weeks to months after surgery until the nerve recovers.
- Some patients may also have a sore throat from the endotracheal (breathing tube) placed during surgery or from the retraction of the esophagus and windpipe during surgery. This tends to get better after surgery.
Dural tear
- The dura is the outer layer of the spinal cord. Sometimes, this layer can be especially thin in certain patients and very friable. During surgery, if there is a small tear in this layer, Dr. Webb will attempt to repair it. This is a not a very common complication, but definitely one that needs to be known.
- Sometimes after a dural tear is repaired, Dr. Webb may ask that you sit upright for 24 hours after surgery. This is done to give the repair time to heal and to ensure his repair does not come apart.
- Fortunately, multiple studies have shown that having a dural tear repair does not affect your outcome from surgery.
Infection
- Very low risk (<1%) but this risk is increased if you are overweight, immunosuppressed, on chronic steroids, or diabetic.
- Antibiotics will be given before surgery starts and also given for 24 hours after surgery while you are in the hospital to decrease the risk of infection.
Bleeding
- Very low risk, but increased if you are taking blood thinners, fish oil, herbal medications or have a clotting disorder.
- These medications will need to be stopped before surgery.
- Sometimes, a special tube called a drain will be placed during surgery. This tube is to collect any blood or fluids that can collect after surgery. This drain will be removed before you leave the hospital, usually the next day after surgery.
Spinal cord or Nerve damage
- Low risk
- A neuromonitoring technician is a professional trained in the monitoring of your nerves and spinal cord.
- This person (along with a Neurologist) is part of the team that will be taking care of you during surgery and will help Dr. Webb monitor your nerves and spinal cord throughout the procedure.
- You will be able to meet this person the morning of surgery and ask any questions about their role in your care.
- Generally, after you are asleep from anesthesia, this technician will place small wires on your legs and arms so that the nerves and spinal cord and be monitored during surgery.
Adjacent Segment Disease:
- Fancy word that means your levels above or below your fusion have degenerated faster because the fused area of the spine places.
- If this occurs and causes symptoms, Dr. Webb will discuss the next steps to manage this starting with conservative treatment options like physical therapy and/or injections.
- A handful of these patients will require additional surgery to address those degenerated levels.