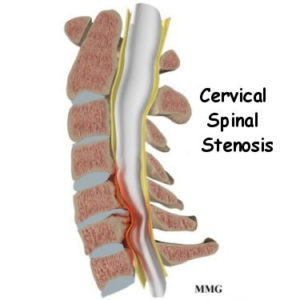
What is Cervical Stenosis?
Cervical stenosis is a condition caused by narrowing of the spinal canal and/or foramen (small openings in the spine that the nerves travel through). Some people are born with a congenitally narrowed spinal canal, but most cervical stenosis occurs when something causes the space that houses the spinal cord and/or nerves to become narrowed.
What causes it?
The leading cause of cervical stenosis is arthritis. Other causes include: herniated discs, overgrowth of bone (bone spurs), thickened ligaments, injuries, or tumors.
What symptoms can it cause?
Cervical stenosis can cause neck pain, radiating arm pain, numbness, weakness, problems with walking and balance, or loss of bladder/bowel control. The radiating pain is sometimes described as pins-and-needles, achy to shock-like, or burning pain which may shoot from your neck all the way down to your fingers. Symptoms can worsen over time.
How can it be treated?
There are generally three levels of treatment that Dr. Webb typically uses to treat patients with cervical stenosis. Some patients, depending on their severity of symptoms, may progress through these levels in an accelerated fashion depending on their reported symptoms and objective physical exam findings. The goals of each level of treatment are to relieve pain and improve function. Most patients can be treated successfully with level 1 or 2 conservative treatment including pain medications, lifestyle modification, injections, and or physical therapy. The remaining patients that fail conservative treatment may require surgical intervention, which is always the final and last resort. Surgery is usually done to remove the compression of the spinal cord and create more space for the nerves to travel.
TREATMENTS
Cervical spinal stenosis can often be treated without surgery. If you start to develop progressive muscle weakness or arm pain, bowel/bladder symptoms, or if you have failed conservative treatments, then surgery may be recommended. Surgery is always the last resort.
Level I – Non-Invasive/Conservative Treatments
- Non narcotic pain medications
- Non-Steroidal Anti-Inflammatories (NSAIDs)
- Oral Steroid Medications
- Physical Therapy, Chiropractic Therapy and/or Home Exercises
- Lifestyle Modification
- Cervical Traction
Level II – Spinal Injections
- Cervical Epidural Injection
- Outpatient procedures
- Done with x-ray guidance
- 1-3 injections may be needed
- Cervical Epidural Injection
Level III – Surgery
Anterior cervical discectomy and Fusion (ACDF)
- Surgery performed by making an incision on the anterior (front) of the neck and the diseased disc + disc herniation are removed. This space is replaced with a plastic or metal cage followed by a plate and screws to fuse that level of the spine. Learn more about ACDF
Cervical Artificial Disc Replacement (ADR)
- Surgery performed by making an incision on the anterior (front) of the neck and the diseased disc + disc herniation are removed. This space is replaced with a metal prosthesis (artificial disc). This procedure has many advantages over a fusion including maintaining motion in that segment of the spine, avoiding advanced degeneration of surrounding levels, and minimizing the chance that you will need further surgery in the future. Learn more about cervical ADR.
Posterior Cervical Foraminotomy
- Surgery is performed by making an incision on the posterior (back) of the neck. Using minimally invasive techniques, the compressing bone and herniation are removed carefully with special instruments. No screws, plates, or hardware are needed. Learn more about posterior cervical foraminotomy.
Posterior cervical decompression and fusion
- Surgery is performed by making an incision on the posterior (back) of the neck and the compressing bone and disc herniation are removed. Screws and rods are usually needed to stabilize the spine. Learn more about posterior cervical decompression and fusion.