What is ACDF?
Anterior is a medical word for “in front”
Cervical is the region of bones that goes from the skull to the bottom of the neck -ectomy is a suffix meaning to remove
Fusion is a surgical technique that joins two or more bones in your spine together to eliminate motion.
So an anterior cervical discectomy & fusion is removing the disc from your neck by going through the front and fusing the bones together so that they don’t move. A fusion usually involves placing a bone graft and metal or plastic implant, where the disc was removed, in order to provide stability and eliminate motion.
Approach
The surgery is done by making a small incision on either the right side or left side of your neck. This will be decided by Dr. Webb and discussed with you at your visit. Doing the surgery by going through the front of your neck has many advantages over going through the back, including:
- Lower infection rate
- Less blood loss
- Less postoperative pain
- Less muscle damage: muscles are not cut, they are moved to the side and allowed to fall back in place when surgery is done.
The Procedure
- Incision
- A skin incision is made on the left or right hand side of the neck. After dissecting through the skin and subcutaneous tissue, Dr. Webb will find the plane between your trachea (windpipe) and esophagus and carefully move these out of the way. No muscles are cut, they are just moved to the side and held apart with the use of special tools, called retractors.
- Performing the Discectomy
- Before removing the diseased disc, Dr. Webb will confirm that he is operating at the correct level by taking an xray while you are asleep.
- When the level is confirmed, Dr. Webb will then begin the decompression portion of the procedure.
- Performing the Decompression
- Dr. Webb will then carefully remove the disc that is pressing on your spinal cord/nerves with the use of special instruments and tools.
- With the intervertebral disc removed, any surrounding structures which may contribute to spinal stenosis are removed as well including bone spurs and excess ligament.
- At times, Dr. Webb will use a microscope so he is able to visualize the smaller anatomical structures with finer detail.
- Performing the Fusion
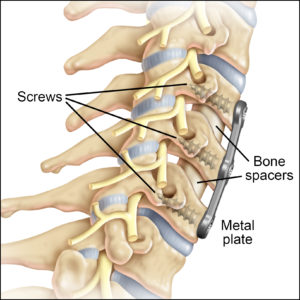
- After the spinal cord has been decompressed and all disc material removed, this area/void needs to be replaced. The area where the disc was removed now gets replaced with bone graft and a metal or plastic cage. This cage will indirectly decompress your spinal nerves by “jacking open” your disc space. This is similar to “jacking up” your car after a flat tire. This cage and graft helps to promote a healing environment that will allow this segment of the spine to fuse together.
- Dr. Webb then uses a small plate with screws in the front to drill into each of the vertebral bones in order to confer stability.
- Closure
- The retractors that held the area between your trachea and esophagus apart will now be removed and the trachea/esophagus will be allowed to fall back into their normal position.
- Dr. Webb will now use absorbable sutures to close your wound. These sutures do not typically need to be removed and will absorb on their own.
- Sometimes, a special tube called a drain will be used. This is to collect any blood or fluids that can collect after surgery. This drain will be removed before you leave the hospital, usually the next day after surgery.
What to expect after surgery
Patients usually spend 1-2 nights in the hospital. During this time, you will be given medications to help with pain and IV antibiotics to minimize the risk of infection. You will be allowed to discharge and go home once your pain is controlled, you are tolerating a diet, and once you are cleared by physical therapy.
Complications
There are risks to any surgery that you should be aware of:
- Inadequate relief of symptoms
- Spinal Injections, done before surgery in the conservative treatment period, are essential in determining which level of your spine is the cause of your symptoms. Inadequate relief of symptoms can be caused by operating on the wrong level of your spine or inadequate decompression of your spine.
- Failure of bone graft to heal adequately (called a non-union or pseudarthrosis)
- If you have diabetes, are a smoker, have been on chronic steroids, or have osteoporosis-you are at risk for a nonunion after surgery. This is when your bones do not fuse after surgery. Dr. Webb will evaluate you for this at each visit and at times will order a CAT scan to evaluate your fusion. Ensuring your blood glucose levels are tightly controlled, smoking cessation, and optimization of your bone health are all critically in reducing the chance that your bones do not fuse together. Some patients whose bones do not fuse may require additional surgery to reattempt a spinal fusion if their symptoms are bad enough to warrant it.
- Nerve damage, causing speech issues
- There are small nerves that control your larynx (voicebox) that reside very close to the surgical site. Dr. Webb carefully works around these nerves and ensures they are not damaged during surgery. If they become irritated by surgery, your voice may be hoarse for weeks to months after surgery until the nerve recovers.
- Dural tear
- The dura is the outer layer of the spinal cord. In some patients, this layer can be very thin and can tear easily. If a tear is encountered during surgery, Dr. Webb will repair it with sutures and enforce this repair with a special glue. At times, Dr. Webb will make you lay flat for 24 hours after surgery to ensure that his repair does not come apart. Fortunately, multiple studies have shown that having a dural tear repair does not affect your outcome from surgery.
- Infection
- Very low risk (<1%), but increased if you are diabetic, overweight, a smoker, are immunocompromised, or if you are a chronic steroid user. You will be given antibiotics before surgery and for 24 hours after surgery to decrease the risk of infection.
- Bleeding
- Very low risk, but increased if you are taking blood thinners, fish oil, herbal medications or have a clotting disorder. Sometimes, a special tube called a drain will be placed during surgery. This tube is to collect any blood or fluids that can collect after surgery. This drain will be removed before you leave the hospital, usually the next day after surgery.
- Spinal cord damage
- Dr. Webb is careful during surgery to ensure that this is minimized. In the operating room during surgery with Dr. Webb will be a Neuromonitoring technician. This is a specialized and trained person who will monitor (along with an offsite Neurologist) your nerves and spinal cord during surgery. You will meet Dr. Webbs neuromonitoring technician in the holding area the morning of surgery.
- Adjacent segment disease:
- This occurs when the levels above or below your fusion begin to degenerate and break down after surgery. A handful of these patients will require additional surgery to address those levels.
“Surgery should only be used as a last and final resort.”
Antonio webb, md